by CAROLYN LEVESQUE
Public Affairs
Pembroke Regional Hospital
EMBROKE – Cancer touches many lives. In Canada alone, an estimated 539 people are diagnosed with cancer each day and it is estimated that two in five Canadians will receive a cancer diagnosis at some point in their lives.
While there’s still no cure, health sector advancements in prevention, screening, diagnosis, treatment, and supportive care are helping ease the burden caused by this disease and Pembroke Regional Hospital is doing all it can to offer a broad range of cancer care services close to home.
Registered Nurse Susan Laderoute who works in Systemic Therapy (chemotherapy) describes the journey her patients go through as an emotional one.
“We see people at their worst and by the end of the first day of treatment they know our first names,” she said. “We become good friends and in many cases we are able to share in their hope as they make plans for the rest of their lives beyond cancer.”
Now in its fifth year at PRH, the fully functioning satellite Systemic Therapy unit, under the auspices of the Ottawa Regional Cancer Centre, has just over 700 visits annually. The local unit treats all solid tumour cancers in new family-oriented space in the hospital’s “D” tower.
In addition to the treatment itself, patient education is done locally. PICC (Peripherally Inserted Central Catheter) service is offered here as is the Chemotherapy Home Infusion Pump Program (CHIPP) for complex bowel cancer. Medical Daycare is available as a support to the unit for such procedures as blood and platelet transfusions, the PRH pharmacy prepares the drugs, a team of highly trained health care professionals are in place, and while patients are here they are under the care of medical oncologists from the Ottawa Regional Cancer Centre who all have privileges at PRH so the care is seamless.
“All our patients are thrilled to receive this care closer to home and the nursing staff here don’t just administer the chemotherapy drugs, we care for the whole person,” Mrs. Laderoute said.
As in most Systemic Therapy units, the end of a treatment regime is marked by the ringing of a special bell.
“It’s an emotional moment when that happens,” she said.
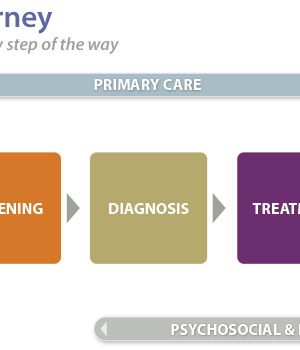
Extending beyond Systemic Therapy, the Pembroke Regional Hospital’s involvement in cancer care is far reaching – with involvement in every aspect of the patient journey from strategic planning and prevention through to palliative care.
Sabine Mersmann, Vice-President of Patient Services – Seniors and Community Care, explains that PRH is one of nine partner hospitals who are part of the Ottawa Hospital Cancer Program, one of 14 regional cancer centres overseen by Cancer Care Ontario.
The purpose of the regional program is to ensure that care is delivered according to province-wide quality cancer standards and to provide care close to home when possible. As part of this, representatives from PRH participate in weekly rounds on the topics of gastrointestinal and breast cancers during which education presentations are made, current research and studies are looked at, regional data is reviewed and more. Tie-ins with the Regional Cancer Centre also mean that our hospital is part of a multi-disciplinary team of surgeons, pathologists, and oncologists who coordinate a standardized way of care.
In terms of screening, Dr. Fred Matzinger, Radiologist and Chief of Diagnostic Imaging, notes that PRH is an affiliate site for the accredited Ontario Breast Screening Program (OBSP) which saw a total of 2,560 exams in 2014/2015.
PRH is also an assessment centre for the workup of screen-detected abnormalities including breast ultrasound, MRI and breast needle biopsy.
In the area of colorectal cancer screening, colonoscopies are performed by surgeons at PRH and CT colonographies (virtual colonoscopies) are performed in the Diagnostic Imaging department for patients who are medically at high risk for colonoscopy or for those who have had an incomplete colonoscopy. In 2014/2015, a total of 2,019 colonoscopies and 276 colonographies took place.
And for cervical cancer screening during the same timeframe, 510 colposcopies were conducted for women who received positive Pap tests.
Moving on to cancer diagnosis, Chief of Surgery Dr. Colleen Haney said that both the diagnosis of cancer and the staging of the disease are routinely performed at PRH using CT or MRI.
“Having the necessary tools available to provide the care needed throughout the cancer journey is key and we are very fortunate in our region to have much of what we need in order to conduct the tests and procedures close to home for our patients at a time when they are vulnerable and scared,” Dr. Haney said.
“Not only are we able to save them a trip or trips to Ottawa, but we are part of a great network that allows us to connect with the cancer specialists very easily and provide the same level of care that our patients would receive anywhere else,” she said.
Dr. Haney said that Image-guided biopsy using ultrasound or CT of all organs (lung, liver, pancreas, breast, lymph nodes, thyroid etc) is also performed at PRH in order to obtain a diagnosis and expedite referral to surgeons and/or oncologists.
Once diagnosed, patients move on to the treatment phase of their journey.
Dr. Haney shared that many cancer surgeries are performed at PRH. In 2014/2015 alone there were 56 breast surgeries and 46 bowel surgeries.
She added that she and the other local surgeons, as well as the radiologists are part of a “Communities of Practice” group for both breast cancer and colorectal cancer disease sites which involves mandatory participation in both weekly rounds via teleconference and quarterly meetings to communicate ongoing updates and develop priorities to provide the best and most coordinated care for patients.
“These linkages provide great opportunities to review successes and areas for improvement, review regional data, develop standardized care pathways and share processes between and within facilities in order to streamline patient access and the patient experience,” Dr. Haney said.
Gynaecologist and Chief of Obstetrics Dr. Siddhartha Mukherjee said that in terms of gynaecological cancers including cervical, endometrial, ovarian and vulvar, much of the diagnosis and treatment of these cases is conducted at PRH in consultation with the Gynaecological Oncology Clinic in Ottawa, with the more invasive types being referred to the clinic.
Much of the follow-up care after cancer surgery and treatment can now be done using telemedicine, which saves patients from the need to travel to Ottawa – excursions which can be costly both time-wise and financially as well as taxing on an individual’s already compromised health.
“In terms of telemedicine availability for cancer care, there has been a lot of growth in the last couple of years,” said Vascular Health Coordinator Karen Roosen.
With between 120 and 200 annual telemedicine visits for follow-up cancer care, Mrs. Roosen said there are currently six regular oncologists who provide follow-up support for all kinds of cancer.
“Patients are very appreciative since most visits are only about 10 minutes,” she said.
Another aspect of cancer care that patients’ express appreciation for is the level of spiritual care shared through our Pastoral Care department.
From time of diagnosis, through hospitalization and other aspects of the journey, emotional support is given and offered in many forms and for those wishing to have religious support regardless of denomination, their needs are met as well.
Compassionate care for patients and their families is also given while supporting end of life in hospital. During this experience, our interdisciplinary team ensures that the patients and their families have access to a comfortable and peaceful environment. Pastoral care provides emotional and spiritual guidance while acknowledging cultural beliefs.
Best practices in pain and symptom management are guided through consultation with the Regional Palliative Care Consultation Team.
Choices are provided to patients and their families about the type of environment and care they would like at end of life. These choices are supported through an integrated team approach representing hospice, home care, palliative care and hospital. During bi-monthly palliative care rounds the team gathers to discuss patient and family care needs in order to facilitate the transition of care between all sites with the common goal being to provide comfort and dignity for persons living with the illness as well as his or her family.
As a member of the Renfrew County Hospice Palliative Care and End of Life Care Network, PRH is directly involved in helping plan for improvements in the regional delivery of palliative care in all settings.
With cancer now recognized as chronic illness, Pierre Noel, hospital president and chief executive officer, acknowledged the importance of a unified, standardized way of care for each and every patient throughout their journey.
“At Pembroke Regional Hospital, our health care team is committed to providing the compassion and high quality care that each cancer patient expects and deserves,” he stated. “Cancer is not a welcome diagnosis for anyone so we do all that we can each step of the way to make the experience as effective and efficient as possible, while keeping as much of their care as possible close to home.”






![Kenopic/Smith Auction [Paid Ad]](https://whitewaternews.ca/wp-content/uploads/2018/10/advertising-100x75.jpeg)

